Mental Health Care Reform
Updated 3/24/10
The Bazelon Center For Mental Health Law participated actively in discussions around health care reform, with the goal of ensuring integration of mental health care in all health plans. On March 21, 2010, the House of Representatives passed the Patient Protection and Affordable Care Act, sending the landmark legislation to the President, who signed it into law two days later. The law is designed to stop discrimination by health insurance companies against those with mental health disorders by establishing parity between them and patients with diseases of the body.
From a letter by Rep. Patrick Kennedy (D-RI): A key aspect of this legislation that is of particular importance to me is the extension of the mental health parity protections established into law last year by my legislation, the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act. Not only are these protections extended to all plans in the Exchange, but mental health and substance use benefits are a part of the essential benefits package created by this legislation. For the 67 percent of adults and 80 percent of children who need mental health care that do not receive it, this victory cannot be understated. Today marks a new day and a giant leap forward towards our transition from a “sick care” system to one which is preventive, collaborative, and patient-centered. |
The statute contains significant improvements in mental health coverage, described in the Bazelon Center's summary. See a congressional review of the law's immediate benefits here.
The next legislative step is consideration by the Senate of a second bill passed by the House, the Reconciliation Act (H.R. 4872) , making changes to the Senate version (see a section-by-section summaryand a House listing of district-by-district benefits).
How will the reform affect you? Interactive pages on The New York Times and The Washington Post explain.
See how your Representative voted:
- Roll call on the Senate bill (H.R. 3590), 219 – 212, which will now go to the President: http://clerk.house.gov/evs/2010/roll165.xml
- Roll call on the Reconciliation Act (H.R. 4872), 220 – 211, which now goes to the Senate: http://clerk.house.gov/evs/2010/roll167.xml
About mental health parity law
Employer-provided health plans have for years routinely set stricter treatment limits and imposed higher out-of-pocket costs on mental health care than care for any other illness. The Mental Health Parity Act of 1996 took a first step toward ending such discriminatory practices and established the principle that mental health benefits should be “on par” with medical and surgical benefits. But the law outlawed only the use of disparate annual or lifetime dollar limits between mental health coverage and coverage of other illnesses. Insurance plans still routinely set arbitrary caps on how many mental-health treatment sessions or days of hospital care they will cover regardless of medical need. And those who “get in the door,” often face far higher out-of-pocket costs than for treatment of any other illness. Congressional efforts to end those discriminatory practices to close the loopholes in the 1996 act have been thwarted for the last six years. The new law closes those loopholes.
US psychiatrist calls for ethics cleanup
CHICAGO — American psychiatrists need to break away from a "culture of influence" created by their financial dealings with the drug industry, the head of the National Institute of Mental Health said in a leading medical journal.
Dr. Thomas Insel stops short of calling researchers corrupt or asking them to stop taking money from drug companies. But he highlights a "bias in prescribing practices" that favors brand names drugs over cheaper generics and non-drug treatments. And he says the situation must change with new standards for transparency and full disclosure of psychiatry's collaborations with industry.
"We can show the rest of medicine how to clean up our act," Insel told The Associated Press. His commentary appears in Wednesday's Journal of the American Medical Association.
His efforts got a boost Tuesday with the signing of the health care overhaul legislation which requires drugmakers and others to file annual reports to the government on their financial ties to doctors. The law requires reporting of gifts, entertainment, food, research money and other fees and grants. Consumer advocates applaud the "sunshine" provision because it also requires a database the public can search for their own doctors' ties to industry.
"Transparency is the first step toward giving patients and the public the tools they need to evaluate those relationships," said Allan Coukell, director of the Pew Prescription Project, a consumer health project of the nonprofit Pew Charitable Trusts.
Current National Institutes of Health rules on financial disclosure are confusing, Insel said. They allow researchers seeking federal funds to make their own judgments about what constitutes a significant financial interest, which they must report to their academic or research institutions. The rules also exempt disclosures of anything below $10,000 annually or 5 percent equity interest in a company. Insel is helping oversee a revision of the NIH's rules, which date back to 1995.
Industry pays for much of the medical research in the United States and many scientists have financial relationships with drug and device makers. Researchers at many institutions are expected to fully disclose those ties to their universities, to the NIH and to the medical journals that publish their research.
Beginning in 2008, an inquiry by Sen. Chuck Grassley, R-Iowa, uncovered millions of dollars in unreported fees paid by drug industry to prominent researchers. The investigation prompted universities and NIH to reassess their conflict-of-interest policies.
When the Grassley inquiry accused seven psychiatrists of failing to report payments they received from drug companies, Insel, himself a psychiatrist, said he tried to determine whether psychiatrists were being targeted unfairly.
He found, instead, evidence that psychiatry may have more drug ties than other medical specialties. In Vermont, for example, which requires public disclosure of industry payments to doctors, psychiatrists receive more money from drug companies than do other types of doctors.
Psychiatric journals report slightly higher rates of industry funding of published studies than other medical journals. And one study found that 90 percent of the advisers who help write American Psychiatric Association guidelines had undisclosed financial ties to industry, Insel writes in JAMA.
Meanwhile, antidepressants and other drug treatments rack up multibillion-dollar annual sales while non-drug treatments such as therapy are "woefully underused," Insel writes.
Insel said he has no financial ties with the drug industry.
Dr. Alan Schatzberg, president of the American Psychiatric Association, told the AP that future leaders of guidelines work groups "will have zero financial relationships with industry during their terms."
Insel's commentary will be influential, said Dr. Emil Coccaro, psychiatry department chairman at the University of Chicago and a recipient of NIH grants.
"It's important that our potential patients and their family members know we're above reproach in terms of undue influence by Big Pharma," Coccaro said.
That's why he threw away all the coffee mugs and pens given to him by drug companies and is careful to report any payments he receives as a board member of a startup biomedical company, he said.



Personality may influence brain shrinkage in aging
Study of aging brains may help in understanding dementia
March 30, 2010
By Tony Fitzpatrick
Psychologists at Washington University in St. Louis have found an intriguing possibility that personality and brain aging during the golden years may be linked.
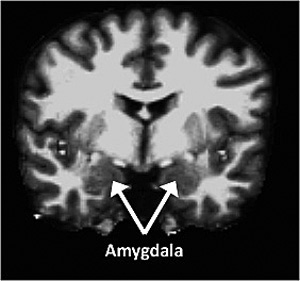
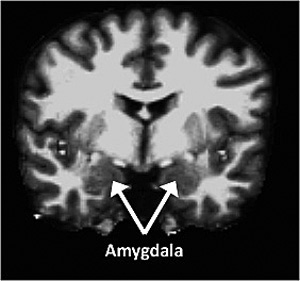
The amygdala, which is part of the medial temporal region and involved in emotion processing, was larger in conscientious individuals but smaller in neurotic individuals
Studying MRI images of 79 volunteers between the ages of 44 and 88 — who also had provided personality and demographic data — the researchers found lower volumes of gray matter in the frontal and medial temporal brain regions of volunteers who ranked high in neuroticism traits, compared with higher volumes of gray matter in those who ranked high in conscientious traits.
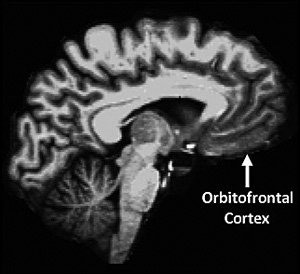
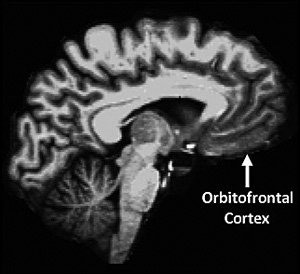
The orbitofrontal cortex, which is part of the prefrontal region and involved in social/emotional processing, showed similar associations with personality.
“This is a first step in seeing how personality might affect brain aging,” says Denise Head, PhD, assistant professor of psychology in Arts & Sciences at Washington University. “Our data clearly show an association between personality and brain volume, particularly in brain regions associated with emotional and social processing. This could be interpreted that personality may influence the rate of brain aging.”
She notes also that the results could be seen as “the tail wagging the dog.” That is, it is actually brain changes during aging that influence personality.

Head
“Right now, we can’t disentangle those two, but we plan to in the future by conducting ongoing studies of the volunteers over time to note future structural changes,” Head says.
Head’s graduate student Jonathan Jackson, first author of a recently published paper on the research in Neurobiology in Aging, says that he, and co-authors Head and David A. Balota, PhD, professor of psychology, tested the hypotheses that aging individuals high in neuroticism would show lower brain volume, while those high in either conscientiousness or extroversion would have larger brain volume. The extroversion results were not clear, but the data validated the other two hypotheses.

Balota
“There are lots of nonhuman animal studies that suggest that chronic stress is associated with deleterious effects on the brain, and this helped us form the hypothesis that we’d see similar effects in older adults.” Jackson says.
“We assumed that neuroticism would be negatively related to structural volume," Jackson says. "We really focused on the prefrontal and medial temporal regions because they are the regions where you see the greatest age changes, and they are also seats of attention, emotion and memory. We found that more neurotic individuals had smaller volumes in certain prefrontal and medial temporal parts of the brain than those who were less neurotic, and the opposite pattern was found with conscientiousness.”

Jackson
“A unique thing that we’ve done is to reliably measure personality differences and associate them with age-related effects on brain structures in healthy middle-aged and older adults” Head says. “Specifically, we found that neuroticism was associated with greater age-related decline in brain volume, whereas conscientiousness was associated with less age-related decline.”
The researchers were interested in healthy aging brains because, down the road, the findings might serve as a useful marker for later diagnosis of dementia. The volunteers they studied are normal control participants at Washington University’s Alzheimer’s Disease Research Center (ADRC), led by John C. Morris, MD, the Friedman Distinguished Professor of Neurology and director of the ADRC.
One of the first changes in Alzheimer's disease may be in personality. There is accumulating research from the ADRC and other institutions that suggest that people tend to become more neurotic and less conscientious in early-stage Alzheimer's.
“It might be that changes in personality track onto those people more likely to develop Alzheimer's,” Jackson says. “It’s why we looked at older healthy adults because it’s important to track these relationships in healthy populations before you look at pathological ones.
"We know that there are degenerative processes going on before the diagnosis of Alzheimer's. We want to be able to see if the subtle personality changes might be particular to an early clinical picture and possibly see if one can predict who will become demented based on personality changes,” Jackson says.
Another way of looking at the findings, Head says, is that neuroticism might add an increasing vulnerability to the pathological processes that go on in aging, particularly in Alzheimer's.
“We will continue to pursue the relationship between personality and brain structure as one of the earlier processes in Alzheimer's and hence a possible risk factor,” Head says.

